Weight loss surgery curbs the sweet tooth by acting on the brain’s reward system, according to a study published November 19 in Cell Metabolism. The researchers found that gastrointestinal bypass surgery, which is used to treat morbid obesity and diabetes, reduced sugar-seeking behavior in mice by reducing the release of a reward chemical called dopamine in the brain. The findings suggest that positive outcomes are more likely if sugary foods seem less rewarding after surgery.
“The problem of how and why bariatric surgery works has been perplexing scientists for years,” says senior study author Ivan de Araujo of Yale University School of Medicine. “By shedding light on how bariatric surgeries affect brain function, our study could pave the way for the development of novel, less-invasive interventions, such as drugs that reduce sugar cravings by preventing sugar absorption or metabolism upon arrival in the gastrointestinal tract.”
Patients, anecdotally, have reported a change in the type of food they preferred after weight-loss surgery. Although the four different operations commonly offered in the United States are effective at reversing obesity and diabetes, it is not entirely clear how these surgeries work. It is likely that there are a number of different mechanisms at play. Bariatric surgeries are more likely to succeed when patients substantially reduce their caloric intake, and reducing sugary foods is an important part of these behavioral changes.
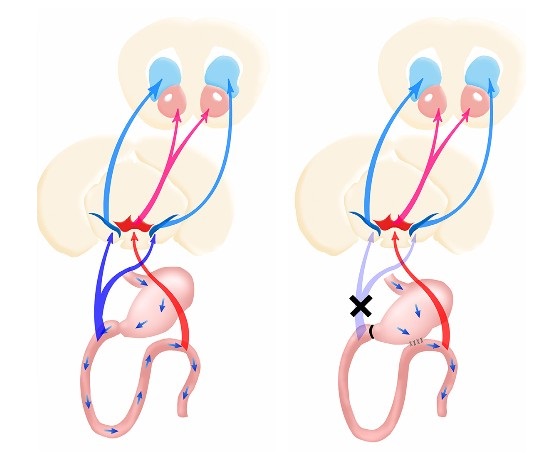
Building on past studies that showed that the brain dopamine reward system regulates caloric intake as well as findings from his team that nutrient sensing in the gastrointestinal tract stimulates dopamine release in the dorsal striatum, de Araujo set out to test whether bariatric surgery relies on the same brain circuitry to curb sugary food preference. They performed surgery in mice to bypass the first part of the small intestine, directly connecting the stomach to a lower section of the gastrointestinal tract. The same procedure is performed in humans, and it mimics the bypass component of the commonly used Roux-en-Y intervention, but no gastric pouch was constructed to limit food intake.
The gastrointestinal rerouting procedure performed in mice suppressed their sweet tooth by reducing sugar-induced dopamine release in the dorsal striatum, essentially diminishing the rewarding effects of sugar. Due to the addictive properties of sweets, infusions of sugar into the stomach would typically cause mice to persistently lick a spout that released a sugary liquid, despite the sensation of fullness. But bypass surgery inhibited the sweet-seeking impulse, almost as if it prevented the sugar addiction from taking hold.
Moreover, using optogenetics, an advanced neuroscience technique, to directly activate the dopamine neural circuit in free-living animals, the researchers saw a striking increase in sugar consumption, overturning the effects of bypass surgery. Mice that underwent this procedure consumed virtually no sweetener following sugar infusions into the stomach, but optical stimulation of the dorsal striatum caused the mice to plant themselves in front of the sugar spout.
“Our findings provide the first evidence for a causal link between striatal dopamine signaling and the outcomes of bariatric interventions,” de Araujo says. “However, we certainly do not want to give the impression that we have an answer for how and why bariatric surgery works. Much more research is needed in this field.”
For his own part, de Araujo plans to directly compare the impact on the brain’s dopamine cells produced by different types of bariatric surgeries. “We hope our work will provide new insights into how different bariatric interventions may lead to a diverse repertoire of behavioral modifications,” de Araujo says. “However, ultimately we would like to help patients lose weight and reverse their diabetes without going under the knife.”
The report, “Striatal Dopamine Links Gastrointestinal Rerouting to Altered Sweet Appetite,” was published online in Cell Metabolism. The work was supported by the National Institutes of Health, the China Scholarship Council, and FAPESP.