Schizophrenia has been known to be associated with a dearth of neural connections in the prefrontal cortex (PFC). The onset of the disease, which often takes place in a person’s early 20s, may be associated with something quite different, however. A joint research team analyzed MRI data from a group of individuals who had recently experienced their first psychotic episode and found that excessive communication within the PFC — rather than a lack of signals — seems to produce abnormal internal states in schizophrenics.

“It is already appreciated by the research community that schizophrenia is likely a ‘dynamic’ neurodevelopmental illness. The reported effects suggest that perhaps following illness onset — which typically occurs in late teens and early 20s — there may be an abnormal elevation in neural activity in certain areas,” Dr. Alan Anticevic, assistant professor of psychiatry at Yale and lead author on the paper, told The Speaker.
The PFC is the frontal lobe of the brain, responsible for higher-order thinking, and has been implicated as a major site of functional impairment in schizophrenia and other severe menal illnesses. Specifically, schizophrenia has been linked in numerous studies with deficits in PFC funcional connectivity, structure and activation.
However, PFC functional connectivity during early-course schizophrenia has not yet been characterized.
The joint Yale-Sichuan University team examined the MRI’s of 129 individuals who had recently undergone their first psychotic episode and who had not yet been medicated.
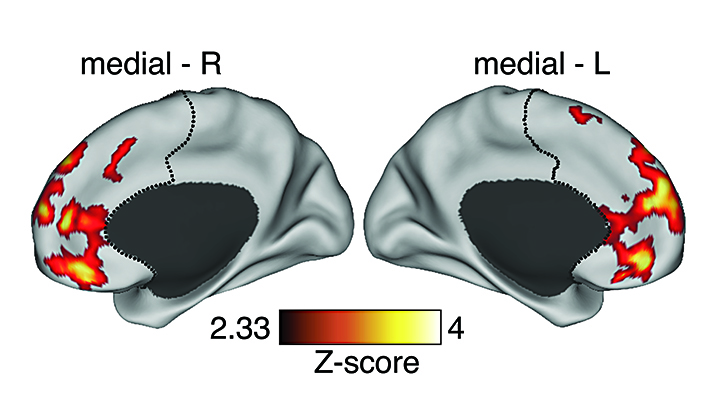
They found evidence of increased PFC connectivity in these patients.
They also tested for hypoconnectivity, and while not finding evidence for this in the PFC, they did detect evidence for hypoconnectivity at the whole-brain level. Generally, the team found, early-course schizophrenia was associated with more severe elevation in PFC connection strength.
“Typically schizophrenia, especially in its more chronic stages, is associated with abnormal reductions in neural activity and connections across the PFC,” Anticevic told us. “The reported effects in part call into question this view by showing that at certain illness stages there seems to be prevailing elevation in PFC connectivity. However, this elevation is likely to be abnormal as it predicted symptoms. This finding may map well onto some emerging theories suggesting that early illness stages may be associated with an abnormal spike in glutamate — a key excitatory neurotransmitter that is present throughout the brain.”

This effect was also captured by a sophisticated mathematical model Anticevic’s group is developing in collaboration with Dr. John Murray at NYU. “This ‘computational psychiatry’ approach helps us to mathematically formalize hypothesized disease mechanisms at the cellular level” Anticevic added. In turn, the team can relate these neurobiologically plausible modeling predictions to their neuroimaging effects.
The team also found that PFC hyperconnectivity normalized for some patients over time, and that this predicted symptom improvement.
Anticevic noted the challenge of attempting to answer the question of what was is happening neurobiologically when PFC hyperactivity is normalized in some individuals diagnosed with schizophrenia in response to treatment, but provided an educated guess.
“We currently don’t have a deep mechanistic understanding of this problem. However, one possibility is that somehow medication is ‘normalizing’ the abnormal elevation in excitation and inhibition balance in local cortical circuits that may be responsible for the hyperactivity. One possible mechanism at the neural system level may involve the interplay of domaine and glutamate between the dorsal striatum and prefrontal cortex, which is the pathway where medication may expert its key effects.”
“We hope to demonstrate that alterations occurring in people who suffer from schizophrenia are likely ‘dynamic,'” concluded Anticevic. “In addition, we hope to demonstrate how the combination of leading neuroimaging approaches and our mathematical models can help us understand these dynamics to develop better therapies for the earliest stages of the illness when intervention is critical.”
The report, “Early-Course Unmedicated Schizophrenia Patients Exhibit Elevated Prefrontal Connectivity Associated with Longitudinal Change,” was completed by Alan Anticevic, Xinyu Hu, Yuan Xiao, Junmei Hu, Fei Li, Feng Bi, Michael W. Cole, Aleksandar Savic, Genevieve J. Yang, Grega Repovs, John D. Murray, Xiao-Jing Wang, Xiaoqi Huang, Su Lui, John H. Krystal, and Qiyong Gong, and was published in the Journal of Neuroscience.
Photos: the Yale-Sichuan University team